Aug. 19, 2020
|
BY Riley Eversull
For more than six months, Naval Medical Center Camp
Lejeune has been battling the COVID-19 pandemic. While epidemiologists
work around the clock to better understand the coronavirus, the medical
center's laboratory technicians, pharmacists, nurses and paramedics must
translate information quickly for their patients and the public.
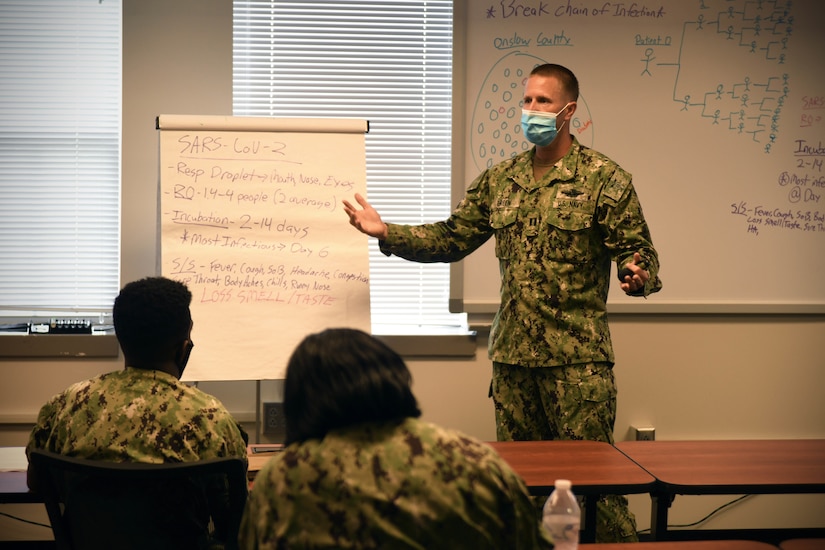
"We pay close attention to lessons learned and best practices
outlined by the Centers for Disease Control and Prevention and
Department of Defense health experts," Navy Lt. Eric Green said,
addressing a recent contact tracing course at Camp Lejeune. "Our contact
tracing has revealed some local trends that we immediately act upon to
educate our forces and beneficiaries, as well as develop our own local
best practices."
Green serves as the medical center's preventive medicine department
head and as assistant public health emergency officer for Marine Corps
Installations East. As COVID-19 took just a matter of weeks to permeate
eastern North Carolina, Green and the preventive medicine department
quickly determined the undeniable need for a team dedicated to tracing
close contacts of COVID-19-positive patients.
"Our team of close contact tracers are working shifts seven-days a
week, 12 or more hours a day, to track down possible close contacts of
confirmed COVID-19 patients," Green said. "Because of the contact
tracing team's hard work, there is an impressive synergy between Marine
Corps operational units [ in Marine Corps Installations East] and local
and state health department officials to thoroughly investigate each
case."
Preventive medicine has hosted a series of contact tracing courses
over the past five months. The most recent course, held on Aug. 5,
brought together medical professionals from Navy and Marine Corps units,
Marine Corps Community Services, child development centers and
Department of Defense Education Activity schools. The class breaks down
what preventive medicine has learned about COVID-19 and the novel, yet
effective, process for tracking close contacts. Class participants can
then take these methods back to their units or organizations to apply to
their daily COVID-19 prevention routines.
"What we are learning is that if you have COVID-19, you could
potentially infect an average of two people, then those two people could
infect four people, and so on," Green said. "People assume because they
aren't showing symptoms right away, they don't have it. However, we are
seeing that the incubation period for COVID is two to 14 days, and by
Day 6 or 7 after exposure – boom. That's often when those symptoms are
hitting, or the symptoms are so mild the person may believe it is just
allergies or the common cold."
To keep close contact tracing operational each week, a team of
Marines from the 2nd Marine Expeditionary Force and Marine Corps Base
Camp Lejeune was trained to aid the contact tracing team. Each morning,
shifts begin in the same manner: dozens upon dozens of phone calls.
"We have six or seven sailors and Marines working each shift, and
these are the guidelines and questions we use when calling possible
close contacts," explains Navy Seaman Demetria Garvin, a hospital
corpsman, as she pulled up a collage of colorful charts and lists on her
computer screen. "We speak directly with the patient, and then we start
contacting individuals that the patient tells us about. We inform them
that they have been identified as a close contact and to self-quarantine
and monitor for symptoms."
Garvin explained that identified close contacts are then called every
24 to 48 hours for symptom checks. When asked what defines a close
contact, Garvin immediately pulled up the most current information on
COVID-19 epidemiology.
"Were you within 6 feet for at least 15 minutes or longer of someone
who has COVID-19?" Garvin said, communicating a couple of the questions
asked of potential close contacts. "Have you had direct physical contact
with someone who has COVID-19?"
If a person is identified as a close contact, contact tracers then
convey the symptoms to monitor. The individual will be advised to remain
home for 14 days to watch for current or possible development of
symptoms. Close contacts are given information on the medical center's
COVID-19 phone help line, the active-duty COVID-19 screening site and
the medical center’s acute respiratory clinic. Contact who notice
symptoms can confer with a medical professional about further testing,
if necessary.
"We want to surround positive cases, isolate them and quarantine
their close contacts," Green said. "The quicker we can do this, the more
effective we can be in stopping an outbreak. What we are seeing is that
we can't necessarily control cases from happening, but we can control
the cluster that comes from cases."
Green described contact tracing as a sort of "box it in" process. In
four steps, personnel are surrounding a COVID-19 case by testing a
patient, isolating the sick, finding close contacts and having patients
quarantine 14 days from the date of exposure.
"So far, we have been effective at controlling the explosive spread
of the virus that we have seen occur throughout other parts of the world
and nation," Green said. "We attribute part of that success to early
and effective contact tracing and getting close contacts into quarantine
quickly before they themselves become infected and subsequently infect
others. It is a tedious and often an imperfect process, but we have
undoubtedly seen these efforts slow the spread of the virus locally."
After more than 100 days spent contact tracing and refining methods,
the contact tracing team has identified what they call avoidable traits,
or the "Big Four," in not contracting COVID-19:
- If you are sick, stay home.
- Avoid large gatherings, especially with people you know to have or possibly have COVID-19.
- If you were a known close contact of someone with COVID-19, self-quarantine for 14 days from the last exposure date.
- If you have a COVID-19 test taken and are waiting for results, isolate at home until you get the results.
Each day, the team reports numbers of positive cases and other
pertinent information to local health departments. While COVID-19 will
not likely disappear soon, Green said, the contact tracing team is not
only helping to "box in" cases, but also is expanding knowledge of how
to prevent falling ill with COVID-19.
"By having this contact tracing process that works, this rapid
response is mitigating further propagation of the disease," he said. "By
doing well at contact tracing, we can flatten our local curve and keep
more people from becoming sick."
What counts as a close contact? Check out these points from the medical center's contact tracing team:
- You were within 6 feet of someone who has COVID-19 for at least 15 minutes.
- You provided care at home to someone who is sick with COVID-19.
- You had direct physical contact with that person (touched, kissed or hugged).
- You shared eating or drinking utensils.
- The person sneezed, coughed or somehow got respiratory droplets on you.
(Riley Eversull is assigned to Naval Medical Center Camp Lejeune.)