Aug. 12, 2020 | , Brooke Army Medical Center
Extracorporeal membrane oxygenation, or ECMO, is a heart-lung bypass intervention that is proving to be lifesaving for some COVID-19 patients.
"ECMO is often the last line of defense for the most critically ill patients with severe pulmonary disease," said Air Force Col. (Dr.) Patrick Osborn, BAMC's deputy commander for surgical services. "Whether due to COVID-19 or another condition, ECMO provides a life-support option that can potentially save lives when all other options are exhausted."
BAMC, one of the few local facilities that offer the treatment, is providing up to one-third of the ECMO capability for the San Antonio area's most severely ill residents, veterans and military beneficiaries suffering from the virus.
"As much as able, BAMC is easing the burden on local health care resources by admitting civilian ECMO patients," Osborn said.
ECMO Explained
This treatment, which requires a multidisciplinary team of specially trained medical personnel, is used in the intensive care unit when a patient experiences heart or lung failure. The ECMO machine removes blood from central vessels in a patient's body, circulates it through an artificial lung, oxygenates it, and delivers the blood back into the bloodstream. In essence, it replaces the natural functions of the heart and lungs, allowing the treatments to help heal the affected organs..
"ECMO is not a treatment for any specific disease," said Air Force Col. (Dr.) Phillip Mason, medical director for BAMC's adult ECMO program. "It works by keeping critically ill patients alive and buying time for us to address their underlying condition. In some cases, we can reduce a patient's chance of dying from 80 to 90 percent down to 30 to 40 percent. While 30 to 40 percent is still high, it represents a significant improvement and translates into many lives saved."
Established in October 2012, BAMC's adult ECMO center is the only one in the Defense Department, and it remains one of the few centers with global air transportable ECMO capability. The multiservice ECMO team has traveled as far as Iraq and Afghanistan to pick up service members in need of the treatment.
While taking care of military beneficiaries is BAMC's primary mission, the organization is able to support civilian ECMO patients through a special Defense Department program. The experience gained ensures the ECMO team sustains the skills required to mobilize worldwide to treat and transport patients back to BAMC, Osborn said.
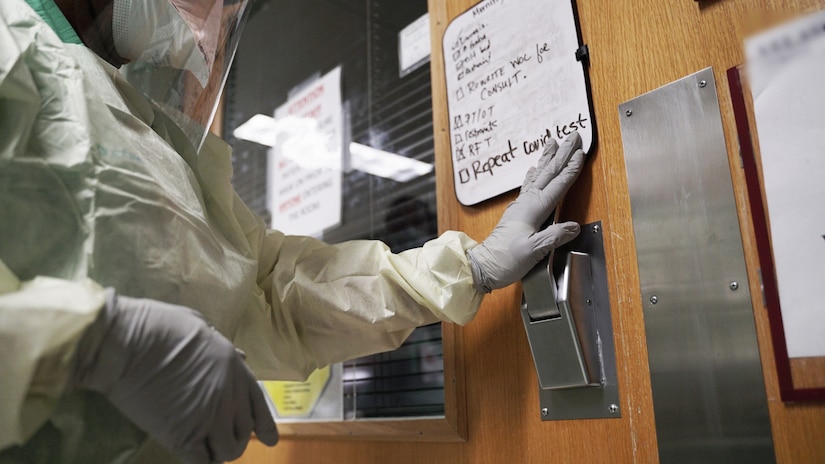
COVID-19 Care
Due to the highly specialized personnel, training and equipment required to care for ECMO patients, BAMC typically could treat only up to four patients at any given time prior to the outbreak. In recent weeks, the hospital has expanded its capability and is treating up to nine patients at a time, most of whom are battling COVID-19.
An ECMO team carefully considers the treatment after other lifesaving measures, such as oxygen therapy or a ventilator, have proven ineffective.
"The vast majority of the critical care community believes that ECMO is effective as a rescue therapy for respiratory failure that does not respond to conventional therapies," Mason noted.
BAMC is also part of a multinational observational trial of ECMO's use for COVID-19. The trial should help to reveal evidence-based proof of the treatment’s effectiveness, but that's further down the line, Mason said.
"While COVID is a complex disease affecting many organ systems, its primary manifestation is respiratory failure, so there is at least some reason to believe ECMO will be effective," he said, noting the treatment is often used for other viral respiratory illnesses, such as influenza.
With the program in place for nearly a decade, BAMC's COVID-19 team is accustomed to working closely with local hospitals in the event a patient may be a candidate for ECMO. This collaboration has stepped up in recent months, creating a larger influx of patients.
To expand capacity to meet the growing community need, BAMC called on its ECMO team to train additional nurses and technicians on the equipment, while also leaning on personnel from the U.S. Army Institute of Surgical Research Burn Center, which is housed in the hospital, to assist.
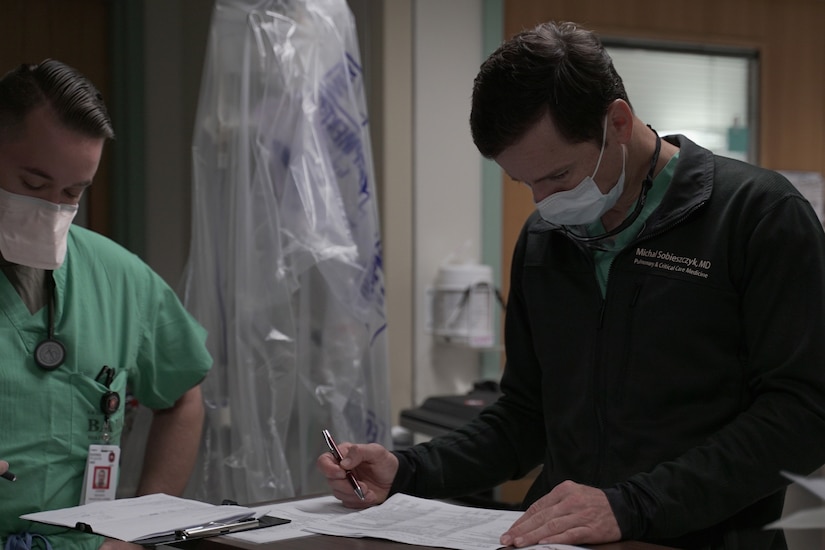
"With the support of the ISR we have been able to expand our ECMO capacity significantly," said Army Maj. (Dr.) Michal Sobieszczyk, staff physician, interventional pulmonology and critical care medicine. "The BAMC and ISR bedside nurses have been instrumental in making the ECMO mission a success."

Lifesaving Treatment
ECMO may be a last resort for COVID-19 patients, but one that has proved lifesaving for many. Sobieszczyk recalled one recent patient in his late 20s who was placed on ECMO twice — once for COVID-19 pneumonia, from which he recovered, and the second time for a bacterial pneumonia and sepsis.
"He required a high level of support and came close to dying several times," Sobieszczyk said. "Fortunately, he was able to be weaned off ECMO and his [breathing tubes were removed] earlier this week."
As a last-resort measure, ECMO is a high-stakes endeavor, Mason noted.
"We have the highest highs and the lowest lows," Mason said. "But each life saved is incredibly rewarding for us and a testament to the importance of this treatment."
ECMO is just one line of defense against COVID-19, but one that BAMC is proud to offer to its beneficiaries and the community, Sobieszczyk said.
"The ECMO team is honored to support the community during this pandemic," he said. "Not only are we able to help the civilian population, but at the same time use this as an opportunity to enhance our mission readiness. It gives everyone a sense of purpose and mission, something we all strive for in the military."
(Elaine Sanchez is assigned to Brooke Army Medical Center.)








No comments:
Post a Comment