By Sarah Marshall Uniformed Services University of the
Health Sciences
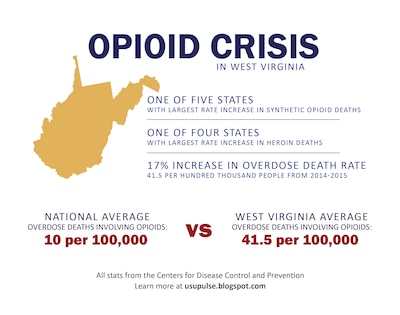
BETHESDA, Md., Aug. 25, 2017 — Opioids are the main driver
of drug overdose deaths across the United States, and West Virginia has been
among the hardest hit by the crisis, experiencing the highest overdose death
rates in the country.
With a shared vision of combating this growing epidemic,
health care providers and researchers from the Uniformed Services University of
the Health Sciences here and West Virginia University have established an
official collaboration to pool their resources.
In 2015, the overdose death rate in West Virginia was an
estimated 41.5 per 100,000 people, an increase of about 17 percent from the
year prior, according to the Centers for Disease Control and Prevention. Cabell
County in southern West Virginia has a population of 96,000, and an estimated
10,000 of those residents are addicted to opioids.
Additionally, the state's indigent burial fund, which helps
families pay for a funeral when they can't afford one, reportedly ran out of
money this year for the sixth consecutive year, largely due to the high number
of overdose deaths.
As the opioid epidemic continues to have a substantial
impact on the state, leaders from WVU reached out to USU's Defense and Veterans
Center for Integrative Pain Management, aware of their efforts to successfully
combat opioid misuse in the military over the last several years with the idea
that lessons learned in the military would be applicable to their state's
current crisis. Earlier this year, leaders from both universities developed a
cooperative research and development agreement allowing them to formally share
pain management resources developed by DVCIPM.
Adding Value to Civilian, Military Medicine
The agreement also allows the DVCIPM an opportunity to
measure the efficacy of the tools they've developed in a new environment – a
collaboration that these leaders believe already is adding value to both
civilian and military medicine.
Nearly a decade ago, at the height of the wars in Iraq and
Afghanistan, physicians were seeking to help troops get their chronic pain
levels to zero as they survived combat injuries in record numbers. This was
often achieved by using opioids – and using opioids as a single modality –
which the military quickly realized was not effective, because this approach
was affecting many service members and their relationships with loved ones,
work, and daily living.
In 2009, then-Army Surgeon General Lt. Gen. (Dr.) Eric
Schoomaker chartered the Army Pain Management Task Force, which sought to make
recommendations for a comprehensive pain management strategy, ensuring an
optimal quality of life for service members and other patients dealing with
pain. It became clear to the military that pain should be viewed as more than
just a number, and over the last several years, the military has been dedicated
to researching and developing more effective tools for pain management,
ultimately reducing the number of those potentially exposed to opioid
addiction.
The task force's efforts led to the development of DVCIPM,
which was designated as a Defense Department Center of Excellence last year.
Schoomaker, now retired, continues to lead these efforts,
serving as vice chair for leadership, centers and programs for USU's department
of military and emergency medicine, which oversees DVCIPM.
"We now have good evidence for the use of
non-pharmacologic, non-opioid treatments, such as yoga, guided imagery, medical
massage, chiropractic, acupuncture, Tai Chi, as well as a closely related
movement therapy called Qigong, and music therapy," he said. "We have
pretty good research to endorse their use."
Because these practices might not work the same for each
person, he added, it's important to use a variety of these modalities as part
of a comprehensive program, tailored to the needs of an individual with chronic
pain. Now, thanks to the official collaboration between USU and WVU, DVCIPM
will have the opportunity to continue researching the efficacy of various
integrative modalities and the pain management tools and resources they've developed.
"We owe it to our patients, and we owe it to
practitioners, to only use tools that have good evidence for their use,"
Schoomaker said.
Gathering, Measuring Data
DVCIPM Director Dr. Chester "Trip" Buckenmaier
said the center's tools and resources have mainly been used in a fairly
selective population within the military. Studying their efficacy in a smaller
system within a state's civilian infrastructure will allow them to gather and
measure data on how successful they can be in a broader population, which will
continue to help illustrate the potential these tools have.
Battlefield acupuncture is a unique auricular (ear)
acupuncture procedure providing an integrative modality to help treat chronic
pain. It’s being taught to qualified providers in the military. Now, thanks to
a new collaboration between Uniformed Services University of the Health
Sciences and West Virginia University, it’s also being employed in a new pain
management center in West Virginia to help combat the opioid crisis. Uniformed
Services University of the Health Sciences photo by Sarah Marshall
"It's important to have relationships like we have with
West Virginia. … They pay off in so many different ways that you can never
anticipate," Schoomaker said.
Dr. Mike Brumage, WVU's assistant dean for Public Health
Practice and Service, initiated the collaborative effort by reaching out to USU
about two years ago, wanting to do something about the issue affecting his
native West Virginia. At the time, he had just retired after a 25-year career
in the U.S. Army Medical Corps, and was able to connect with former military
health colleagues, including Schoomaker and then-Army Maj. Gen. (Dr.) Richard
Thomas, who was serving as the Defense Health Agency's chief medical officer.
Thomas is an alumnus of WVU's undergraduate, dental and medical programs, and
is now USU's president.
This quickly led to several more meetings and discussions,
led by Dr. Clay Marsh, vice president and executive dean of WVU's Health
Sciences Center, and Dr. Bill Ramsey, assistant vice president of coordination
and logistics for the center.
Ultimately, they arrived at a CRADA, signed off by Thomas and Marsh, and
have since continued looking for ways to make the most out of their
collaboration.
The hope is that this joint effort will galvanize further
interest from other entities, Schoomaker said, leading to other similar
collaborations, ultimately continuing the fight against a crisis that's impacting
the entire nation.








No comments:
Post a Comment